Cutaneous aspergillosis in an immunocompetent patient: a case report
Bagate A.1, Birare S.2, Jadhav D.3, Nalpe V.4, Patekar D.5*
DOI: https://doi.org/10.17511/jopm.2020.i02.14
1 A.N. Bagate, Department of Pathology, S.R.T.R. Govt., Medical College, Ambajogai, Maharashtra, India.
2 S.D. Birare, Department of Pathology, S.R.T.R. Govt. Medical College, Ambajogai, Maharashtra, India.
3 D. S. Jadhav, Department of Pathology, S.R.T.R. Govt. Medical College, Ambajogai, Maharashtra, India.
4 Vinay Nalpe, Department of Pathology, S.R.T.R. Govt. Medical College, Ambajogai, Maharashtra, India.
5* Divya Patekar, Department of Pathology, S.R.T.R. Govt. Medical College, Ambajogai, Maharashtra, India.
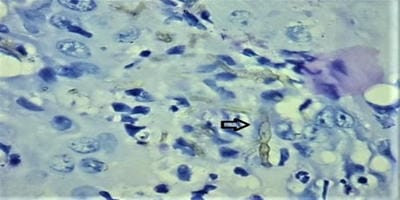
Cutaneous aspergillosis is a rare disease that is usually seen in immunosuppressed patients. It is rarely found in immunocompetent patients and it is mostly caused by Aspergillus. flavus, Aspergillus fumigatus, and rarely by Aspergillus niger. Cutaneous Aspergillosis is of two types: primary or secondary. Primary cutaneous aspergillosis frequently involves sites of skin injury, at or near intravenous catheter sites, at sites associated with occlusive dressings, at sites of traumatic inoculation, surgery or burns. Secondary cutaneous lesions occur as a result of either from widespread blood-borne seeding of the skin or it may occur from contiguous extension to the skin from an infected underlying structure. The current study is presenting a case of a 25-year-old female, a farmer by occupation, presented with multiple scaly plaques and verrucous nodules with a past history of trauma over knee 3 years back. After trauma she initially noticed lesions over knee followed by the elbow, face and oral lesions noticed 7 months back. There was no present or past history of weight loss, anorexia and serological tests were negative for HIV. One year back she was diagnosed as lupus vulgaris and received Anti-Tubercular treatment without much benefit. She came to our hospital where biopsy from lesions over elbow revealed dense inflammatory exudate, septate fungal hyphae showing acute angle branching on H and E stain and PAS stain, which is suggestive of aspergillosis. Scrapping from oral lesion also revealed inflammatory cells with septate fungal hyphae with acute angle branching on PAP stain. Histopathological, cytological study and fungal culture show fungal infection caused by Aspergillus niger.
Keywords: Cutaneous aspergillosis, Immunocompetent patient, Aspergillus. Flavus, Immunosuppressed
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Department of Pathology, S.R.T.R. Govt. Medical College, Ambajogai, Maharashtra, India. Email: |
Bagate AN, Birare SD, Jadhav DS, Nalpe V, Patekar D. Cutaneous aspergillosis in an immunocompetent patient: a case report. Trop J Pathol Microbiol. 2020;6(2):204-209. Available From https://pathology.medresearch.in/index.php/jopm/article/view/445 |


 ©
©