A comparative study of Pap smear cytology and histopathology of cervix biopsy
Selvanayaki K.1, Archana A.2*
DOI: https://doi.org/10.17511/jopm.2020.i03.04
1 K.M. Selvanayaki, Associate Professor, Annapoorna Medical College and Hospital, Salem, Tamil Nadu, India.
2* Archana Archana, Associate Professor, Dhanalakshmi Srinivasan Medical College and Hospital, Perambalur, Tamil Nadu, India.
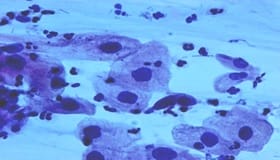
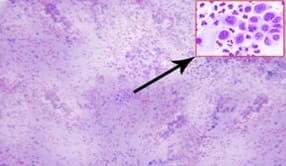
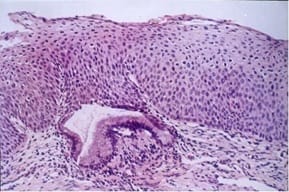
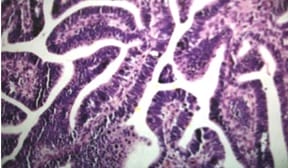
Background: Carcinoma cervix is one of the leading causes of death of the female population in developing countries. By virtue of its accessibility, cancer of the cervix can be readily diagnosed even in its preinvasive stage. If treated in the earlier stages the patient can often be cured of the disease. Carcinoma of the cervix is the fourth most frequent cancer in women worldwide and the leading cause of death from cancer in several developing countries including India. The use of cervical smear (Papanicolaou/Pap) as a screening tool has significantly reduced the incidence of cervical cancer. Materials and Methods: The present study was carried out in the department of pathology in a tertiary care hospital over a period of two years. In the two year study period, 2568 pap smears were received. Among these, 194 abnormal smears were identified and they were categorized under The Bethesda System 2014. The histopathological examination of biopsy cervix results of the smears was compared and analyzed. Results: Out of 194 smears studied, reactive changes was 69 (35.57%). Atypical squamous cells of undetermined significance were 47 (24.23%). Low grade squamous intraepithelial lesions were 3 (1.55%) and high grade squamous intraepithelial lesions were 29 (14.95%). Atypical endocervical cells were 2 (1.03%). Atypical endocervical cells favor neoplastic was 4 (2.06%) and endocervical adenocarcinoma in situ was 1 (0.5%). Squamous cell carcinoma was 39 (20.10%). The histopathological examination of biopsy cervix results of the above smears was compared and analyzed. Conclusion: This correlative study of Pap smear and histopathological examination of the cervix revealed the overall sensitivity of 97%, the specificity of 74% and an accuracy of 87%. The false-negative and false-positive cases in this study can be minimized by proper sampling, screening, interpretation and further follow up study of repeat smears.
Keywords: Carcinoma cervix, Cervical smear, Pap smear cytology
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Associate Professor, Dhanalakshmi Srinivasan Medical College and Hospital, Perambalur, Tamil Nadu, India. Email: |
Selvanayaki KM, Archana A. A comparative study of Pap smear cytology and histopathology of cervix biopsy. Trop J Pathol Microbiol. 2020;6(3):230-237. Available From https://pathology.medresearch.in/index.php/jopm/article/view/440 |


 ©
©