A demographic study of a series of eosinophilic appendicitis and its correlation with the clinicopathological profile in a tertiary care hospital-a 3-year study
Padmavathy K.1*, Arumugam VG.2, Illavarasan E.3, Srinivasan V.4
DOI: https://doi.org/10.17511/jopm.2020.i02.08
1* Karthika Padmavathy, Department of Pathology, Sri Muthukumaran Medical College and RI, Chennai, Tamil Nadu, India.
2 Vasugi Gramani Arumugam, Department of Pathology, SRIHER, Chennai, Tamil Nadu, India.
3 Elakkiya Illavarasan, Consultant, Humain Health Clinic and Lab, Chennai, Tamil Nadu, India.
4 Vijayalakshmi Srinivasan, Department of Pathology, Sri Muthukumaran Medical College and RI, Chennai, Tamil Nadu, India.
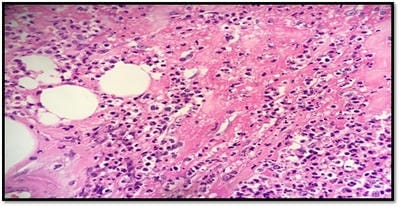
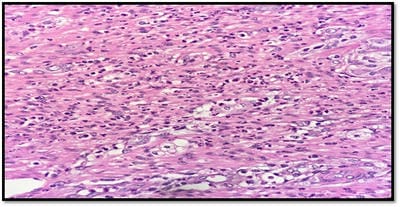
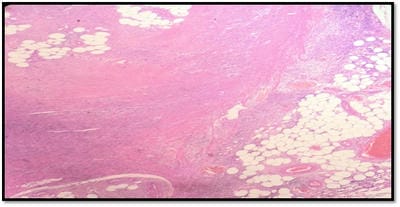
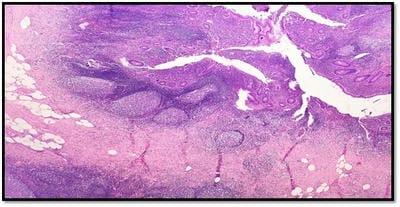
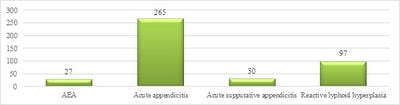
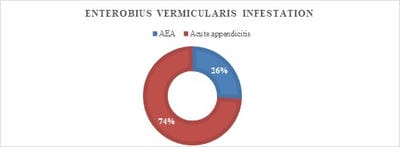
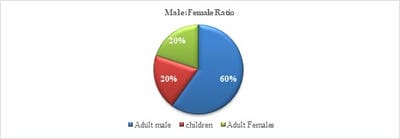
Introduction: Acute eosinophilic appendicitis (AEA) is a rare variant of inflammation of the appendix. The histologic hallmark of this entity is the infiltration of eosinophils in the musularis layer of the appendix with edema separating the muscle fibers with very few or no neutrophilic infiltration. A retrospective study was done to determine their demographic profile, morphological diagnosis, and clinical correlation. Materials and Methods: All cases of Acute appendicitis reported at the histopathology department of Sri Muthukumaran Medical College and Research Institute, a teaching hospital from the year of Jan 2017 to Dec 2019 were included in this study. Histopathological examination is the gold standard for the diagnosis of acute appendicitis. Hence, Formalin-fixed paraffin-embedded tissue which was stained with Hematoxylin and Eosin were retrieved and used for routine morphology and diagnosis. Results: Out of 419 cases of appendicectomies studied, 27 (6.49%) cases were found to be acute eosinophilic appendicitis, 265 (63.7%) cases were acute appendicitis, 30 (7.2%) cases were reported as acute suppurative appendicitis with periappendicitis most of which showed infiltration of eosinophils along with other inflammatory cells and 97 (23.3%) cases were reported as appendix with reactive lymphoid hyperplasia. Conclusion: It was inferred that the acute eosinophilic appendicitis is a condition which could be an allergic response and an early event in the evolution of acute phlegmonous appendicitis.
Keywords: Appendicitis, Eosinophilic, Allergic response
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Department of Pathology, Sri Muthukumaran Medical College and RI, Chennai, Tamil Nadu, India. Email: |
Padmavathy K, Arumugam VG, Illavarasan E, Srinivasan V. A demographic study of a series of eosinophilic appendicitis and its correlation with the clinicopathological profile in a tertiary care hospital-a 3-year study. Trop J Pathol Microbiol. 2020;6(2):161-166. Available From https://pathology.medresearch.in/index.php/jopm/article/view/424 |


 ©
©