A study of liquid-based cytology in cervical smears
Phani Meghana B.1, Venkata Renuka I.2, Ramya C.3*, Durga Prasad B.4, Sireesha K.5
DOI: https://doi.org/10.17511/jopm.2020.i03.05
1 Bolla Phani Meghana, Postgraduate, Department of Pathology, NRI Medical College and Hospital, Vijayawada, Andhra Pradesh, India.
2 Inuganti Venkata Renuka, Professor and Head of Department, Department of Pathology, NRI Medical College and Hospital, Vijayawada, Andhra Pradesh, India.
3* Chitturi Ramya, Assistant Professor, Department of Pathology, NRI Medical College and Hospital, Vijayawada, Andhra Pradesh, India.
4 Baddam Durga Prasad, Postgraduate, Department of Pathology, NRI Medical College and Hospital, Vijayawada, Andhra Pradesh, India.
5 Kolla Sireesha, Postgraduate, Department of Pathology, NRI Medical College and Hospital, Vijayawada, Andhra Pradesh, India.
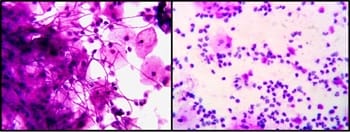
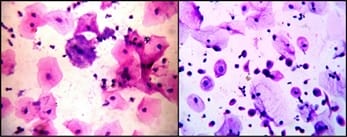
Introduction: Cervical cancer is a major health problem. It ranks second in mortality affecting the world population. Cervical cancer has the advantage that it takes a long time for it to develop. During this time it can be diagnosed and treated properly. For this purpose pap smears (cervical smears) are routinely screened for pre-malignant lesions using Liquid Based Cytology. Purpose: The purpose is to study the prevalence of cervical lesions by EZI PREP method and to determine the prevalence of cervical lesions in various age groups. Material and Methods: This was a prospective study done in the Department of Pathology. All the data regarding the patient was recorded in a predefined proforma. Results: A total of 1500 cervical smears were taken into the study. The age group of females ranged from 20-80 years. All the satisfactory smears were evaluated. Inflammatory smears, infectious smears, and smears with epithelial cell abnormalities were identified in the present study. Conclusion: Out of the 1500 LBC smears studied, the majority (1134) of the smears studied were inflammatory. Epithelial cell abnormalities were found in 21 cases and the most common age group of epithelial abnormalities was the fifth decade.
Keywords: Epithelial cell abnormalities, EZI PREP, Liquid-based cytology, Pap smear
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Pathology, NRI Medical College and Hospital, Vijayawada, Andhra Pradesh, India. Email: |
Meghana BP, Renuka IV, Ramya C, Baddam DP, Kolla S. A study of liquid-based cytology in cervical smears. Trop J Pathol Microbiol. 2020;6(3):238-244. Available From https://pathology.medresearch.in/index.php/jopm/article/view/422 |


 ©
©