A rare mesentric tumor "paraganglioma" - a case report
Gidwani N.1*, Jain N.2, Agarwal S.3
DOI: https://doi.org/10.17511/jopm.2020.i01.16
1* Nikita Gidwani, Final Year Resident, Department of Pathology, Mahatma Gandhi Medical College and Hospital, Jaipur, Rajasthan, India.
2 Niharika Jain, Final Year Resident, Department of Pathology, Mahatma Gandhi Medical College and Hospital, Jaipur, Rajasthan, India.
3 Sonia Agarwal, Associate Professor, Department of Pathology, Mahatma Gandhi Medical College and Hospital, Jaipur, Rajasthan, India.
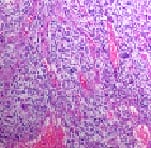
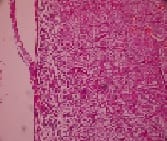
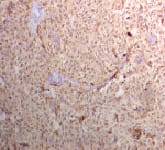
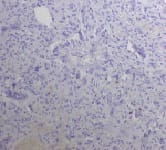
Paraganglioma are rare type of neuroendocrine tumors that arise from embryonal neural crest. Paraganglioma of adrenal medulla is known as Pheochromocytoma. Extra adrenal localization has incidence of 2-8 per million people per year, which can extend from upper cervical region to pelvis related to autonomic nervous system. Even rarer is occurrence of paragangliomas outside the usual distribution of paraganglionic tissue. Mesenteric paragangliomas are extremely rare. The present case was of a non-functional extra adrenal paraganglioma occurring in a 43-year-old male presented with complain of pain in abdomen and mild discomfort. Abdominal CECT revealed well defined enhancing solid mass with central necrosis in right side of mesentry. Explorative laparotomy and surgical excision were done, on histology typical "zellballen" pattern was found. Paragangliomas are rare neuroendocrine tumor known to store and secrete catecholamines and hence are known as functional paragangliomas and may present with symptoms like headache, sweating, palpitations and hypertension.
Keywords: Paraganglioma, Intra-Abdominal surgery, Abdominal surgery, Neuroendocrine cells, Immunohistochemistry
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Final Year Resident, Department of Pathology, Mahatma Gandhi Medical College and Hospital, Jaipur, Rajasthan, India. Email: |
Gidwani N, Jain N, Agarwal S. A rare mesentric tumor "paraganglioma" - a case report. Trop J Pathol Microbiol. 2020;6(1):98-102. Available From https://pathology.medresearch.in/index.php/jopm/article/view/418 |


 ©
©