Evaluating the spectrum of histomorphological patterns on endoscopic biopsy in patients with upper gastrointestinal tract disorders
Theresa J.1, Lavanya M.2, Rakesh J.3*, Basha K.4
DOI: https://doi.org/10.17511/jopm.2020.i01.01
1 J. Margaret Theresa, Assistant Professor, Department of Pathology, Sri Venkateshwaraa Medical College Hospital and Research Centre, Pondicherry, Puducherry, India.
2 Lavanya M., Associate Professor, Department of Pathology, Sri Venkateshwaraa Medical College Hospital and Research Centre, Pondicherry, Puducherry, India.
3* J. Gerard Rakesh, Associate Professor, Department of Pathology, Sri Venkateshwaraa Medical College Hospital and Research Centre, Pondicherry, Puducherry, India.
4 K. Sultan Basha, 2nd year MBBS Student, Department of Microbiology, Sri Venkateshwaraa Medical College Hospital and Research Centre, Pondicherry, Puducherry, India.
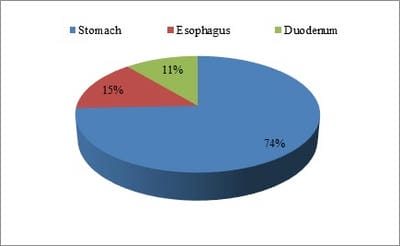
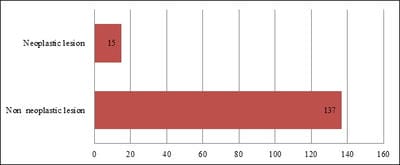
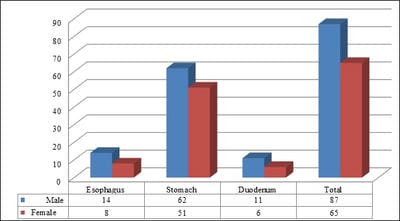
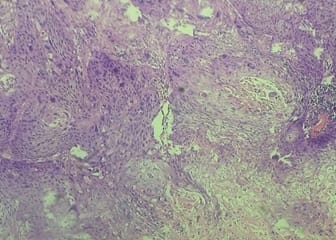
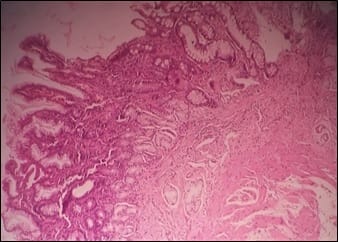
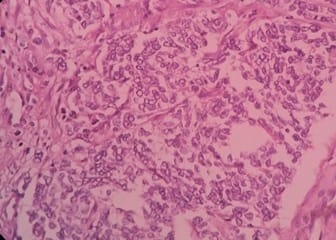
Introduction: The upper gastrointestinal tract (UGT) disorders are more common complaints in clinical practice and have got high degree of mortality and morbidity. Many different types of lesions can affect the upper gastrointestinal tract and can be classified as congenital anomalies, infections, inflammation and neoplastic lesions. Material and Methods: A total of 152 cases of upper gastrointestinal tract biopsies are included in this study, out of which 113 cases were gastric biopsies, 22 cases were esophageal biopsies and the remaining 17 cases were duodenal biopsies. Present study was carried out in the Department of Pathology at Sri Venkateshwaraa Medical College Hospital and Research Centre, Puducherry for a period of one year between March 2018 and February 2019. All the biopsies were performed using fiberoptic endoscopy. Results: It is reported among 152 cases of UGT biopsies 137 were non-neoplastic lesions and 15 were neoplastic. Commonly affected age group was 31-40 years followed by 41 to 50 years. As per the present study, males were affected more predominantly than females. Out of the 22 cases from esophageal biopsies, 16 cases showed non-neoplastic lesions and 6 were neoplastic.
Keywords: Gastrointestinal tract disorders, Endoscopic Biopsy, Histomorphological examination, Helicobacter pylori, Malignant neoplasms and Squamous cell carcinoma
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Associate Professor, Department of Pathology, Sri Venkateshwaraa Medical College Hospital and Research Centre, Pondicherry, Puducherry, India. Email: |
Theresa MJ, Lavanya M, Gerard RJ, Sultan BK. Evaluating the spectrum of histomorphological patterns on endoscopic biopsy in patients with upper gastrointestinal tract disorders. Trop J Pathol Microbiol. 2019;6(1):1-8. Available From https://pathology.medresearch.in/index.php/jopm/article/view/401 |


 ©
©