material was aspirated in 9 patients (56.2 %), pus was aspirated in 2 patients (12.5%), while whitish material and mucoid material were aspirated in one patient each (6.2 %). Both patients in whom pus was aspirated had a tender swelling. FNAC was repeated in 3 patients.
The microscopic findings of FNAC are shown in Table 2. Ziehl-Neelsen (ZN) staining was done in all patients and only 1 patient was positive for AFB. In one patient culture report from aspirated material showed mycobacterium species.
Table-2: Microscopic findings upon FNAC.
| Microscopy of salivary gland shows |
No. of cases (% of cases) |
| Epithelioid cell granuloma |
16 (100%) |
| iant cells |
8 (50 %) |
| Necrosis |
3 (18.8 %) |
| Neutrophils |
3 (18.8 %) |
| Acinar cells |
6 (37.5 %) |
| Ductal cells |
2 (12.5 %) |
Anti-tubercular treatment (ATT) was given in 5 patients, all of whom showed improvement after the treatment. Therefore, 5 out of the total of 16 cases were most likely to be tuberculous parotitis (31.2 %), while 12 cases had granulomatous diseases other than tuberculosis. In 1 patient, the parotid swelling reduced completely after antibiotic treatment for 5 days.
Discussion
Tuberculosis is a major health problem, especially in developing countries. However, tuberculosis of salivary glands is a rare variety of extrapulmonary tuberculosis. Tuberculosis of salivary glands is rare because of the bactericidal effect of salivary enzymes [2]. The pathogenesis of parotid tuberculosis remains unclear. The parotid gland and its lymph nodes can be involved by two mechanisms. Firstly, as a result of a focus of mycobacterial infection in the oral cavity (infected tooth, tonsil or sputum). Secondly as a result of hematogenous or lymphatic spread from a distant primary lung focus [1,4-6]. In the present study, swellings in 3 patients were associated with lymphadenopathy. The most commonly implicated agent is Mycobacterium Bovis and rarely by atypical mycobacteria [6].
Lee and Liu described the clinicopathological features of tubercular parotitis based on a study of 49 cases of tubercular parotitis [7]. Two clinical forms of tubercular parotitis have been described.
Acute tuberculous sialadenitis usually presents with diffuse glandular enlargement and is often painful. In the present study, 3 cases had painful enlargement of the parotid gland. Chronic sialadenitis manifests as an asymptomatic localized lesion within the parotid gland, which slowly keeps growing in size for many years [4]. This mimics a neoplasm [2]. It may also present as pre-auricular fistula and in advanced cases, facial nerve involvement [2,8]. The differential diagnosis includes malignancy of the parotid gland, mumps, sarcoidosis, and actinomycosis. A total of 25 % of patients with parotid tuberculosis have a concomitant pulmonary infection [1,2].
Parotid tuberculosis becomes a real diagnostic problem in the absence of clinical lung disease and without any systemic symptoms or signs of tuberculosis [2]. A chest radiograph may be helpful in cases of associated pulmonary tuberculosis. The use of erythrocyte sedimentation rate and tuberculin skin testing (PPD) can provide valuable information but requires an initial suspicion [1]. One of our cases had slightly raised ESR. Similarly, ESR was raised in the case report by Sharma T et al. [9]. Apart from the presence of non-caseating granulomas, elevated angiotensin-converting enzyme levels and a negative Mantoux test favor a diagnosis of sarcoidosis over other granulomatous lesions [9].
FNAC is an easy and reliable outpatient procedure for the diagnosis of tubercular parotitis, and it is ideally suited for use in resource-limited settings, especially in developing countries. FNAC has a sensitivity of 81-100 % and specificity of 94-100 % in the diagnosis of parotid tuberculosis [10]. A total of 20.6 % of FNAC are non-diagnostic; which could be due to the complexity of tissue architecture. However, this can be overcome by doing a repeat FNAC. Also, in the case of active infection, the FNAC report may be inconclusive [11]. FNAC was repeated in 3 out of 16 patients in the present study.
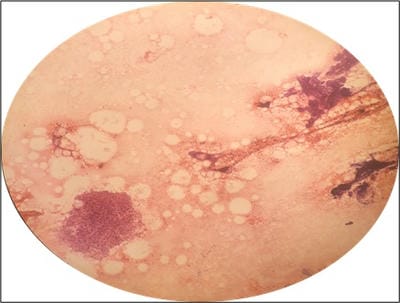
In the current study, FNACs of 38.1 % of the patients showed granulomatous inflammation (Figure 1) and at least 11.9% of the swellings were likely due to tuberculosis. This is more as compared to the study by Van Der Walt et al in which 12.1% of the swellings showed granulomatous inflammation and only 1.9% of these swellings were due to tuberculosis [11]. This difference could be due to a lesser prevalence of tuberculosis in western countries.


 ©
©