Leiomyosarcoma of the tongue: A case report
Gahlot A.1*, Zaheer S.2
DOI: https://doi.org/10.17511/jopm.2020.i03.08
1* Adwaita Gahlot, Department of Pathology, Vardhman Mahavir Medical College, New Delhi, India.
2 Sufian Zaheer, Department of Pathology, Vardhman Mahavir Medical College, New Delhi, India.
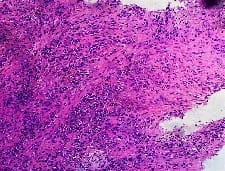
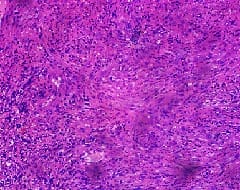
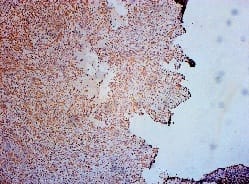
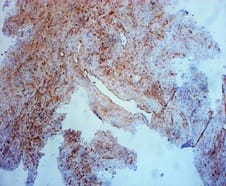
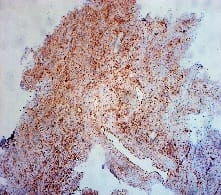
Leiomyosarcoma (LMS) of the tongue is an extremely rare malignant mesenchymal tumor. Visceral lesions are the most common and account for about 7% of all soft-tissue sarcomas. The lesion is rare in the head and neck, making up 3%–10% of all leiomyosarcomas. Primary leiomyosarcoma of the tongue is extremely rare leiomyosarcomas andrepresents 5–6% of all soft tissue sarcomas and usually, they arise in the uterus, gastrointestinal tract, and retroperitoneum. The most common sites of head and neck regions are the oral cavity (22%), the sinonasal tract (19%), and the facial skin-subcutis (17%). Smooth muscle tumors in the oral cavity usually arise from the buccal mucosa, the gingiva, and the oral floor,but only a few numbers of cases arise in the tongue.The present case shows the tumor cells arranged in fascicles and interlacing bundles. The nuclei of individual tumor cells are elongated and hyperchromatic with a moderate amount of eosinophilic cytoplasm. The tumor cells were strongly positive for immunoreactivity with Vimentin, and SMA. However, CK, P63, EMA, desmin, CD99, and S100 were negativefrom these immunohistochemical results, the pathological diagnosis was leiomyosarcoma at the tip of the tongue.The tumor cells were strongly positive vimentin and SMA. However, CK, P63, EMA, desmin, S100, and CD99 were negative. From these immunohistochemical results, the pathological diagnosis was leiomyosarcoma, left side of the tongue.
Keywords: Tongue, leiomyosarcoma, SMA
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Department of Pathology, Vardhman Mahavir Medical College, New Delhi, India. Email: |
Gahlot A, Zaheer S. Leiomyosarcoma of the tongue: A case report. Trop J Pathol Microbiol. 2020;6(3):261-264. Available From https://pathology.medresearch.in/index.php/jopm/article/view/391 |


 ©
©