Seroprevalence and trends in transfusion transmitted infections in blood donors: a 6-year experience in a tertiary care hospital
Bagde S.1, Tiwari AK.2*, Behera TR.3, Bombeshwar V.4, Indoria C.5
DOI: https://doi.org/10.17511/jopm.2020.i01.03
1 Sadhna Bagde, Associate Professor, Department of Pathology, Government Medical College, Rajnandgaon, Chhattisgarh, India.
2* Amit Kumar Tiwari, Assistant Professor, Department of Pathology, Government Medical College, Rajnandgaon, Chhattisgarh, India.
3 Tapas Ranjan Behera, Resident, Department of Hematology and Medical Oncoloy, Cleveland Clinic, , Ohio, United States of America.
4 Vikash Bombeshwar, Demonstrator, Department of Pathology, Government Medical College, Rajnandgaon, Chhattisgarh, India.
5 Chandrashekhar Indoria, Assistant Professor, Department of Pathology, Government Medical College, Rajnandgaon, Chhattisgarh, India.
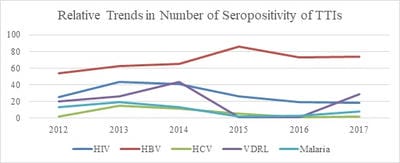
Introduction: Blood transfusion continues to be a possible source of pathogens in transfused patients. The pattern of transfusion-transmitted infections (TTI) varies between regions. Knowledge of prevalence of TTIs is essential to monitor safety of blood transfusion by ensuring better practices of collection and processing of blood components. The aim of the study was to determine the prevalence of TTI in blood donors in a tertiary care hospital in central India. Materials and Methods: A retrospective cross sectional study was performed from 2012 to 2017 in a tertiary care government hospital in central region of India. The study analyzes all voluntary and replacement blood donations received through the hospital in its blood bank and blood donation camps organized by the hospital. Results:A total of 54,831 units of blood was collected over a period of 6 years. Prevalence of TTI in the blood donors was 1.45%. Prevalence of seroprevalence of human immunodeficiency virus (HIV), hepatitis B virus (HBV), hepatitis C virus (HCV), syphilis and malaria were 0.31 %, 0.75%, 0.065%, 0.22% and 0.1% respectively. Among all the potential donors, the most common TTI prevalence was that of Hepatitis B followed by HIV and syphilis. Conclusion:Public awareness, careful donor selection,vigilant screening and adoption of newer techniques for inactivation of pathogens are needed to ensure safety of blood products and their transfusion.The public outreach programs such as blood donation camps could be used as a way of spreading awareness to improve the safety and efficacy of a blood donation program.
Keywords: Blood donor, Infection, Prevalence, Transfusion-transmitted infections
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Pathology, Government Medical College, Rajnandgaon, Chhattisgarh, India. Email: |
Bagde S, Tiwari AK, Behera TR, Bombeshwar V, Indoria C. Seroprevalence and trends in transfusion transmitted infections in blood donors: a 6-year experience in a tertiary care hospital. Trop J Pathol Microbiol. 2020;6(1):18-22. Available From https://pathology.medresearch.in/index.php/jopm/article/view/389 |


 ©
©