Spectrum of various skin nodule mimicking cutaneous adnexal tumour
Samanta M.1, Saini SK.2*, Mathur D.3, Mangal N.4, Vyas K.5, Dubey A.6
DOI: https://doi.org/10.17511/jopm.2020.i01.06
1 Matariswa Samanta, Assistant Professor, Department of Pathology, Pacific Institute of Medical Sciences, Udaipur, Rajasthan, India.
2* Seemant Kumar Saini, Assistant Professor, Department of Pathology, Pacific Institute of Medical Sciences, Udaipur, Rajasthan, India.
3 D.R. Mathur, Professor, Department of Pathology, Pacific Institute of Medical Sciences, Udaipur, Rajasthan, India.
4 Nitesh Mangal, Assistant Professor, Department of Community Medicine, Pacific Institute of Medical Sciences, Udaipur, Rajasthan, India.
5 Komi Vyas, Assistant Professor, Department of Pathology, Pacific Institute of Medical Sciences, Udaipur, Rajasthan, India.
6 Anshita Dubey, Tutor, Department of Pathology, Pacific Institute of Medical Sciences, Udaipur, Rajasthan, India.
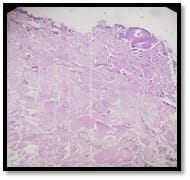
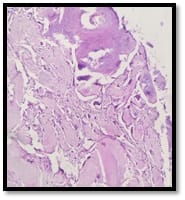
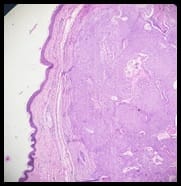
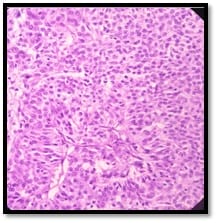
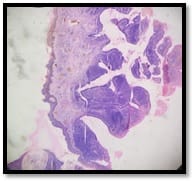
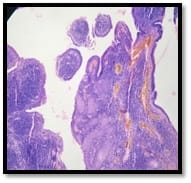
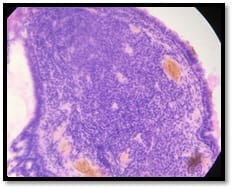
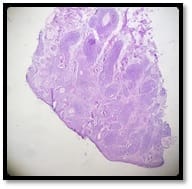
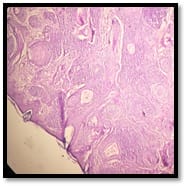
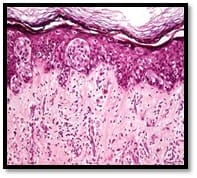
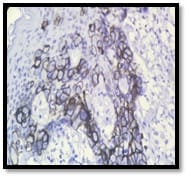
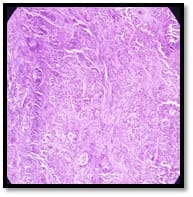
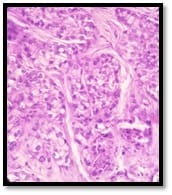
Introduction: Cutaneous adnexal tumors are the group of uncommon tumour usually misdiagnosed clinically with various soft tissue tumour. Therefore, histopathology is the gold standard to diagnose their histogenesis. The aim of the present study is to find out the occurrence of skin adnexal tumors according to age, sex and site distribution along with histopathological diagnosis. Materials and Methods: This retrospective study was conducted in Department of Pathology of Pacific Institute of Medical sciences, Udaipur from September 2016 to August 2019. The formalin fixed paraffin embedded tissue section was stained with hematoxylin and eosin stain for microscopical analysis. Results: A total number of 41 adnexal tumors out of which 22 males and 19 females were studied out of which 36 cases were diagnosed as benign and 5 cases were reported as malignant. The most common cutaneous adnexal tumors diagnosed as sweat gland origin followed by hair follicle, sebaceous gland and pagets disease of nipple. Majority of the cutaneous adnexal tumors reported in head and neck site in a fourth to sixth decades of life. Conclusion: Architectural features help us to diagnose different types of cutaneous adnexal tumors.
Keywords: Cutaneous adnexal tumours, Sweat gland, Histopathology
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Pathology, Pacific Institute of Medical Sciences, Udaipur, Rajasthan, India. Email: |
Samanta M, Saini SK, Mathur DR, Mangal N, Vyas K, Dubey A. Spectrum of various skin nodule mimicking cutaneous adnexal tumour. Trop J Pathol Microbiol. 2020;6(3):35-42. Available From https://pathology.medresearch.in/index.php/jopm/article/view/379 |


 ©
©