Role of Fine Needle Aspiration Cytology in Effective Management of Patients with Granulomatous Inflammation in Neoplastic and Non-Neoplastic Lesions
Patel D.1*, Shukla A.2, Jivani T.3
DOI: https://doi.org/10.17511/jopm.2021.i03.06
1* Drashti Patel, Senior Resident, Department of Pathology, Surat Municipal Institute of Medical Education and Research, Surat, Gujarat, India.
2 Ashwini Shukla, Professor (Additional), Department of Pathology, Surat Municipal Institute of Medical Education and Research, Surat, Gujrat, India.
3 Toral Jivani, Assistant Professor, Department of Pathology, Surat Municipal Institute of Medical Education and Research, Surat, India.
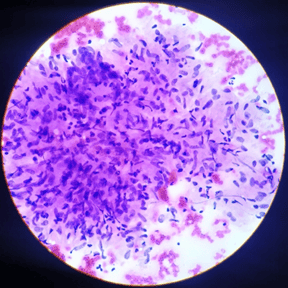
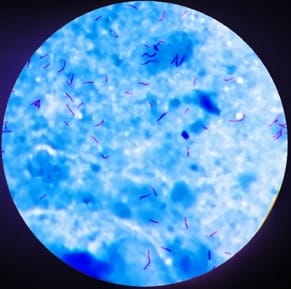
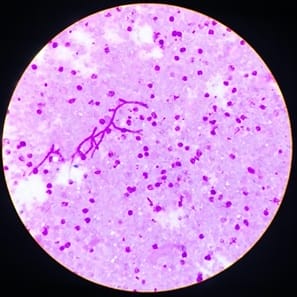
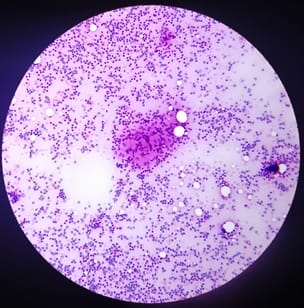
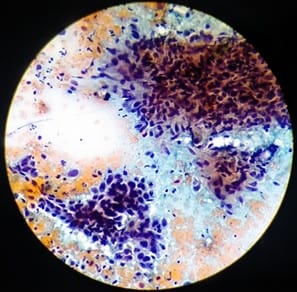
Background: Granulomatous inflammation is a common diagnosis given in fine-needle aspiration cytology (FNAC) and it is a type of chronic inflammation in which tissue reaction appears following cell injury. Aims: To assess the usefulness of the cytological study in the diagnosis of granulomatous lesions. Materials and Methods: An observational study is done based on cytomorphological evaluation of 156 cases of granulomatous inflammation diagnosed at the Department of Pathology, in Surat Municipal Institute of Medical Education & Research over 18 months from February 2018 to July 2019. Results: Out of the total of 156 cases of granulomatous inflammation, tuberculosis was the most common finding in 111 cases (71.15%), followed by fungal infection (05 cases). The male to female ratio was 1.0 to 1.4. The most commonly affected age group was 21 to 30 years. Conclusions: All the cases of granulomatous inflammations are analysed for definitive diagnosis to provide early and proper treatment of underlying diseases, malignancies or lymphoma.
Keywords: Fine needle aspiration cytology, Granuloma, PAS stain, Tuberculosis, ZN Stain
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Senior Resident, Department of Pathology, Surat Municipal Institute of Medical Education and Research, Surat, Gujarat, India. Email: |
Patel D, Shukla A, Jivani T. Role of Fine Needle Aspiration Cytology in Effective Management of Patients with Granulomatous Inflammation in Neoplastic and Non-Neoplastic Lesions. Trop J Pathol Microbiol. 2021;7(3):128-134. Available From https://pathology.medresearch.in/index.php/jopm/article/view/530 |


 ©
©