Fine needle aspiration cytology of thyroid lesions: A single-centre experience
Sheikh S.1, Abbas F.2, Beigh A.3, Farooq S.4*, Latief M.5
DOI: https://doi.org/10.17511/jopm.2021.i02.04
1 Sheema Sheikh, Associate Professor, Department of Pathology, Government Medical College, Srinagar, Jammu and Kashmir, India.
2 Farhat Abbas, Senior Resident, Department of Pathology, Government Medical College, Srinagar, Jammu and Kashmir, India.
3 Ambreen Beigh, Medical officer, Department of pathology, Government Medical College, Srinagar, Jammu and Kashmir, India.
4* Summiya Farooq, Assistant Professor, Department of Pathology, Government Medical College, Srinagar, Jammu and Kashmir, India.
5 Muzamil Latief, Senior Resident, Department of Nephrology, Government Medical College, Srinagar, Jammu and Kashmir, India.
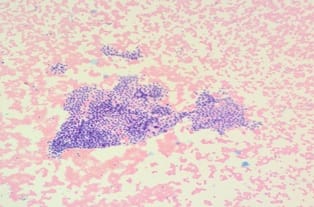
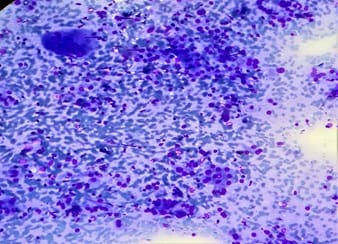
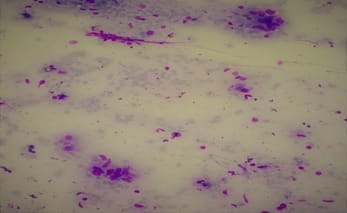
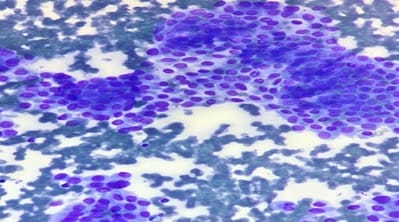
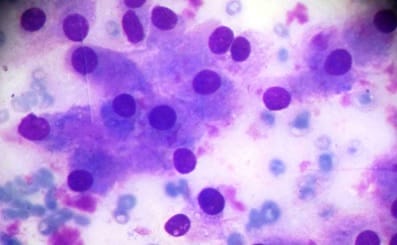
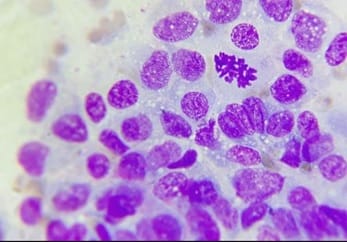
Background FNAC (Fine needle aspiration cytology) is an easy and cost-effective method for the diagnosis of thyroid lesions. The use of the Bethesda system is largely helpful in eliciting the risk of malignancy and helps in further management of patients with thyroid lesions. In this study we studied thyroid lesions and reported them according to the BETHESDA System of Classification based on cytological features on FNAC. Materials and Methods: In this prospective single-centre study conducted over 2 years we included 642 patients with thyroid lesions who underwent FNAC. These lesions were then classified according to the Bethesda system based on cytomorphological features. Results: Out of 642 patients included in our study, 100 were males and 542 were females with a male: female ratio of 1:5.42. The age of the patient population in our study ranged from 4-94 years. Among 642 cases in our study most (61.38%) cases were benign whereas 9.96% cases were found to be malignant and 2.60% cases were suspicious of malignancy. Conclusion: Bethesda System of reporting FNAC of thyroid lesions is a standardized system and helps in deciding diagnostic approach and appropriate management of patients.
Keywords: FNAC, Thyroid, Bethesda system, Cytology
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Pathology, Government Medical College, Srinagar, Jammu and Kashmir, India. Email: |
Sheikh S, Abbas F, Beigh A, Farooq S, Latief M. Fine needle aspiration cytology of thyroid lesions: A single-centre experience. Trop J Pathol Microbiol. 2021;7(2):85-92. Available From https://pathology.medresearch.in/index.php/jopm/article/view/524 |


 ©
©