The utility of fine-needle aspiration cytology in differentiating granulomatous mastitis and tuberculous mastitis
Sukumar C.1, Singh G.2*, Kumar Yadav S.3, Jahan A.4, Singh S.5, Sarin N.6
DOI: https://doi.org/10.17511/jopm.2021.i01.04
1 Challa Sukumar, DNB Resident, 2* Garima Singh, Specialist, 3 Shakti Kumar Yadav, Senior Resident, 4 Aarzoo Jahan, GDMO-II, 5 Sompal Singh, Specialist, 6 Namrata Sarin, Specialist and Head of the Department; all authors affiliated with the Department of Pathology, North Delhi Municipal Corporation Medical College and Hindu Rao Hospital, Delhi, India.
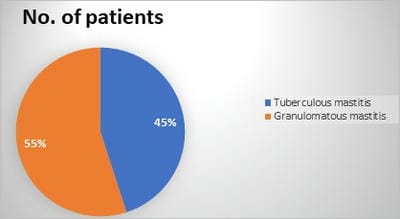
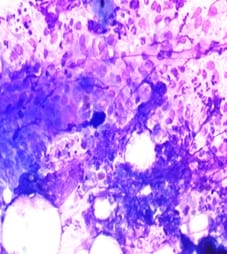
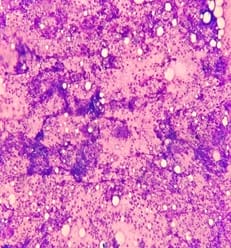
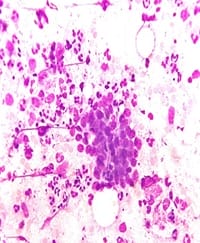
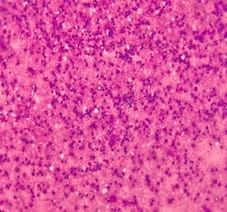
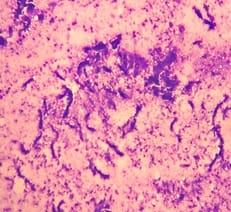
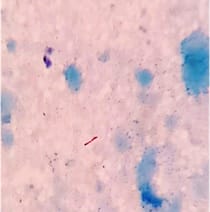
Background: Tuberculous mastitis (TM) is a rare extrapulmonary presentation of tuberculosis accounting for less than 1% of all diseases of the breast in the industrialized world. Granulomatous Mastitis (GM) is an uncommon chronic inflammatory disease of the breast that almost always mimics cancer in young individuals, so it can be a diagnostic dilemma. Aims and objectives: The main aim of this study is to elucidate the utility of FNAC in differentiating granulomatous mastitis and tuberculous mastitis. Materials & Methods: A retrospective observational study was conducted at the department of pathology, Hindu Rao Hospital, Delhi. Cytology database was revealed for a period of 4 years (2016-2019). The clinical details wherever available and cytological morphology of individual cases were noted and analysed. Results: In our study out of 20 cases 11 cases (55%) were found to be granulomatous mastitis and the other 9 cases (45%) were found to be tuberculous mastitis. All cases were of female patients only, with equal side distribution. In the cytological smears of GM, three (27.3%) smears showed ductal epithelial cells, epithelioid cell granulomas were seen in 11 (100%) cases and singly scattered epithelioid cells were seen in nine (81.8%) cases. Caseous necrosis was observed only in one case (9.09%) but necrotic material intermixed with degenerated neutrophils and apoptotic bodies were seen in four cases (36.4%). Conclusion: FNAC can be an accurate method for differentiating tuberculous mastitis from granulomatous mastitis as per cytomorphological findings, along with confirmation by the demonstration of acid-fast bacilli and hence can help to decide the appropriate treatment protocols for such patients.
Keywords: Tuberculous Mastitis, granulomatous mastitis, Fine needle aspiration (FNAC), Acid-fast bacillus (AFB), Epithelioid cell granulomas
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Specialist, Department of Pathology, North Delhi Municipal Corporation Medical College and Hindu Rao Hospital, Delhi, India. Email: |
Sukumar C, Singh G, Yadav SK, Jahan A, Singh S, Sarin N. The utility of fine-needle aspiration cytology in differentiating granulomatous mastitis and tuberculous mastitis. Trop J Pathol Microbiol. 2021;7(1):26-32. Available From https://pathology.medresearch.in/index.php/jopm/article/view/500 |


 ©
©