Scrotal abscess with xanthogranulomatous epididymo-orchitis: a case report of rare diagnostic entity
Verma R.1, Dalal N.2*, Yadav A.3, Pawar R.4, Singh S.5
DOI: https://doi.org/10.17511/jopm.2020.i07.04
1 Renuka Verma, Assistant Professor, Department of Pathology, Pandit Bhagwat Dayal Sharma Post Graduate Institute of Medical Sciences, Rohtak, Haryana, India.
2* Niti Dalal, Senior Resident, Department of Pathology, Pandit Bhagwat Dayal Sharma Post Graduate Institute of Medical Sciences, Rohtak, Haryana, India.
3 Archana Yadav, Resident, Department of Pathology, Pandit Bhagwat Dayal Sharma Post Graduate Institute of Medical Sciences, Rohtak, Haryana, India.
4 Richa Pawar, Assistant Professor, Department of Pathology, Pandit Bhagwat Dayal Sharma Post Graduate Institute of Medical Sciences, Rohtak, Haryana, India.
5 Sunita Singh, Senior Professor, Department of Pathology, Pandit Bhagwat Dayal Sharma Post Graduate Institute of Medical Sciences, Rohtak, Haryana, India.
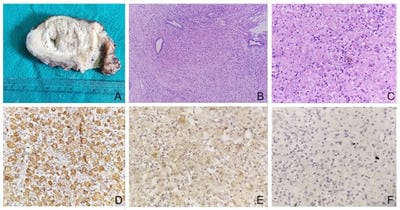
Xanthogranulomatous epididymo-orchitis is an extremely rare diagnostic entity presenting as a scrotal mass with or without pain. Rarely, it can affect prostate, epididymis, and testicle. It can mimic a testicular malignancy both clinically as well as radiologically, hence, careful pathological examination and biomarker study are essential to rule out malignancy. We report a case of 50 years old male with increasing right testicular swelling with a discharging pus. Skin over scrotum was gangrenous. Right orchidectomy was performed. Histopathological diagnosis revealed features of xanthogranulomatous epididymo-orchitis with no evidence of malignancy. IHC markers for tumor were negative.
Keywords: Xanthogranuloma, Epididymitis, Orchitis, Malignancy
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Senior Resident, Department of Pathology, Pandit Bhagwat Dayal Sharma Post Graduate Institute of Medical Sciences, Rohtak, Haryana, India. Email: |
Verma R, Dalal N, Yadav A, Pawar R, Singh S. Scrotal abscess with xanthogranulomatous epididymo-orchitis: a case report of rare diagnostic entity. Trop J Pathol Microbiol. 2020;6(7):443-445. Available From https://pathology.medresearch.in/index.php/jopm/article/view/486 |


 ©
©