Desmoplastic Infantile Astrocytoma and Desmoplastic Infantile Ganglioglioma – not so infantile anymore
Sahai J.1*, Sahu S.2
DOI: https://doi.org/10.17511/jopm.2020.i07.05
1* Jyotsna Sahai, Resident, Department of Pathology, MGM Medical College and Hospital, Navi Mumbai, Maharashtra, India.
2 Shilpi Sahu, Professor and HOD, Department of Pathology, MGM Medical College and Hospital, Navi Mumbai, Maharashtra, India.
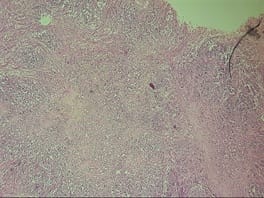
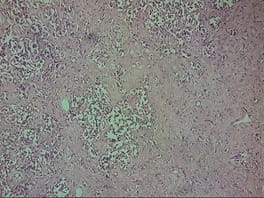
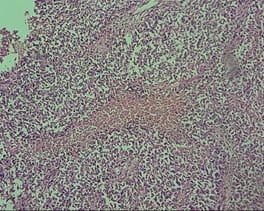
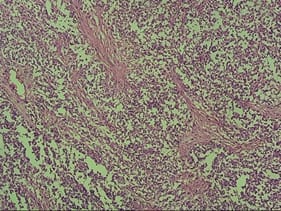
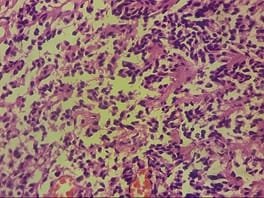
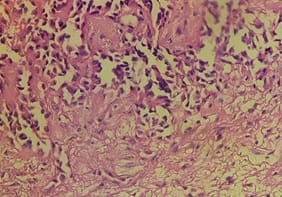
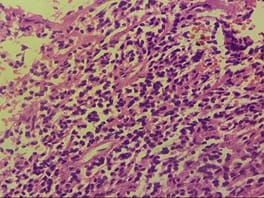
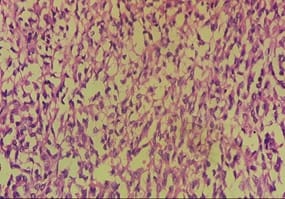
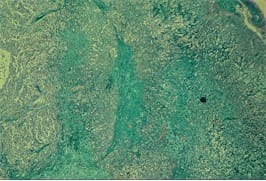
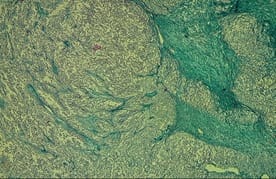
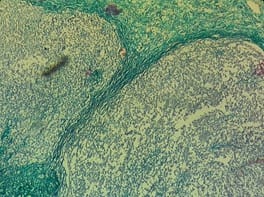
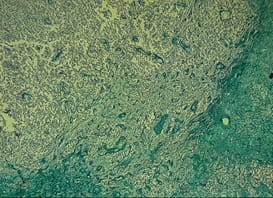
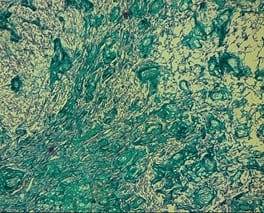
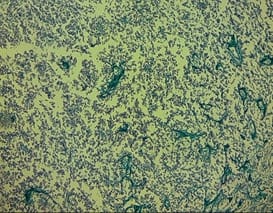
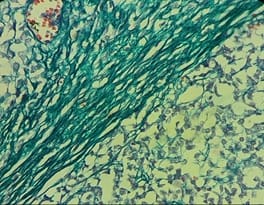
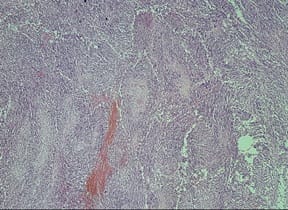
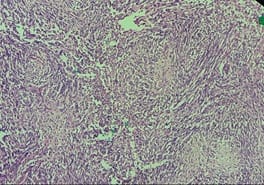
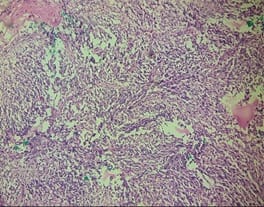
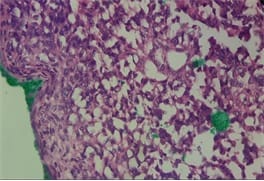
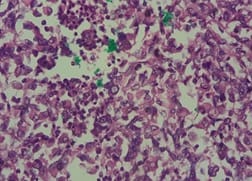
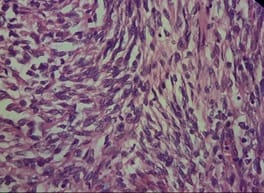
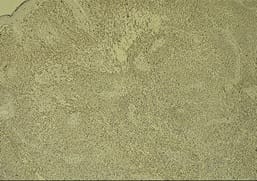
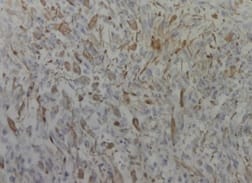
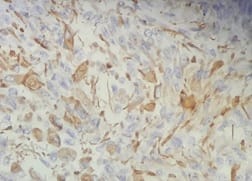
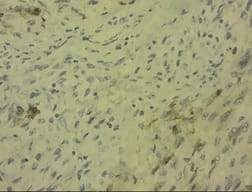
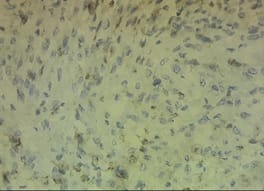
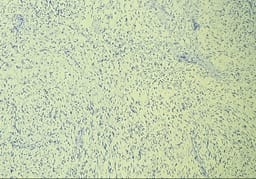
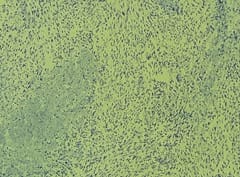
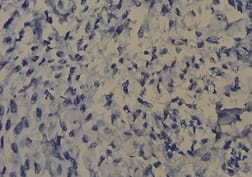
DIA and DIG are rare, infantile, supratentorial neoplasms that usually occur in children before 2 years of age and are exceedingly rare in older age groups. They appear as hypodense, cystic masses with solid components showing dural attachment on neuroimaging. They are characterized by reticulin-rich spindle cell stroma containing connective tissue due to meningeal involvement, microscopically. These tumors have potential for misdiagnosis because they contain varying proportions of neoplastic glial, neuronal and poorly differentiated cells, which causes them to have a “small round blue cell tumor” like appearance, though they have a good prognosis if correctly diagnosed. The current study report two cases diagnosed at our institution that had very late presentation with varying complaints which challenged the normally believed dictum of these tumors being entirely infantile.
Keywords: Astrocytoma, CNS, Desmoplastic, Ganglioglioma, Infantile, Tumor
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Resident, Department of Pathology, MGM Medical College and Hospital, Navi Mumbai, Maharashtra, India. Email: |
Sahai J, Sahu S. Desmoplastic Infantile Astrocytoma and Desmoplastic Infantile Ganglioglioma – not so infantile anymore. Trop J Pathol Microbiol. 2020;6(7):446-454. Available From https://pathology.medresearch.in/index.php/jopm/article/view/485 |


 ©
©