Study of the hematological scoring system and C-reactive protein (CRP) in determining Neonatal sepsis
Ramesh Godbole C.1*, Ramdas Joshi S.2, Jaison J.3
DOI: https://doi.org/10.17511/jopm.2020.i02.11
1* Chandrahas Ramesh Godbole, Associate Professor, Department of Pathology, MIMER Medical College, Talegaon, Maharashtra, India.
2 Sneha Ramdas Joshi, Professor and Head of Department, Department of Pathology, MIMER Medical College, Talegaon, Maharashtra, India.
3 Janice Jaison, Associate Professor, Department of Pathology, MIMER Medical College, Talegaon, Maharashtra, India.
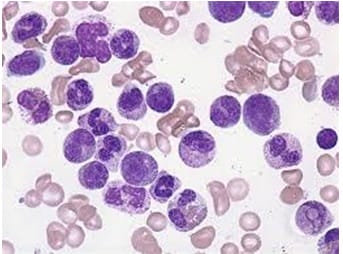
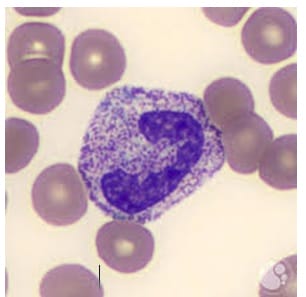
Background: Laboratory sepsis markers play an important role in the assessment of a neonate with clinical signs of a probable infection with. C - reactive protein (CRP), Blood culture (BC), Hematological Scoring System (HSS) are three well-identified parameters designated for the investigation of Neonatal Sepsis or infection. Material and Methods: The current study was a prospective hospital-based cross-sectional study carried out at the Department of Pathology, MIMER Medical College, Talegaon (D), Maharashtra, India. Neonates with features suggestive of sepsis and Neonates with recent maternal infection were included in the study. Sensitivity, specificity, Positive Predictive Values (PPVs) and Negative Predictive Values (NPVs) were calculated for each parameter. Results: A total of 40 neonates suspected of having sepsis were enrolled in the current study. In the current study, blood culture was positive in 10 cases (25%), out of which 6 (60%) were Gram-positive and 4 (40%) were Gram-negative, whereas 30 cases were found to be negative for blood culture. The mean CRP levels in positive culture cases were 85.7±17, whereas, in the negative culture case, the mean CRP Levels were 38.7±23, whereas the mean value in control was 5.88±0.72. Conclusion: HSS is a simple, easy, cheap, and rapid adjunct for the diagnosis of clinically suspected cases of neonatal sepsis. C-reactive protein values correlate well with HSS in predicting sepsis. However, C-reactive protein does not have any advantage over HSS, either as a single test or in combination.
Keywords: Neonatal sepsis, C - reactive protein (CRP), Blood culture (BC), Hematological Scoring System (HSS)
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Associate Professor, Department of Pathology, MIMER Medical College, Talegaon, Maharashtra, India. Email: |
Godbole RC, Joshi SR, Jaison J. Study of the hematological scoring system and C-reactive protein (CRP) in determining Neonatal sepsis. Trop J Pathol Microbiol. 2020;6(2):181-190. Available From https://pathology.medresearch.in/index.php/jopm/article/view/446 |


 ©
©