lymphocytes, and immunoblasts. Suppurative lymphadenitis was diagnosed by the presence of sheets of neutrophils. Necrotic lymphadenitis was marked by extensive areas of necrosis. Ziehl-Nelson stain was used for finding AFB.
Tuberculosis was diagnosed when AFB was positive. Microfilaria was also searched for in lymph node aspirate. Non-Hodgkin's lymphoma was diagnosed by the presence of a monomorphic population of lymphocytes scattered singly in a highly cellular smear and the absence of RS cell.
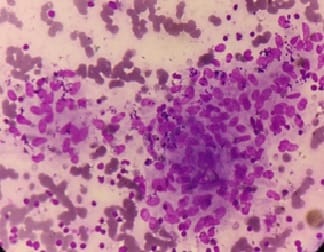
Diagnosis of Hodgkin’s lymphoma (Figure-2) was made on the basis of the presence of either mononuclear Hodgkin’s cells or Classical RS cells in the background of lymphocytes, eosinophils, plasma cells, and histiocytes. Metastatic deposits were diagnosed by the presence of cytological patterns and cellular details.
Age and sex- In the present study, the age of the patients ranged from 2 to 79 years. Most of the cases belonged to the age group of 21-30 years. There were 63.2% males and 36.8% females resulting in male: female ratio of 1.72:1.
In the study done by Badge et al, it was seen that age of the patients ranged from 2.5 to 87 years. The youngest patient was diagnosed as tubercular lymphadenitis, and the oldest patient was diagnosed as having metastatic deposits in the lymph node from a squamous cell carcinoma. The majority (74.3%) of the patients were in the age group of 11–50 years, with a peak in the age group 21-30 years. Only 15 patients were aged <10 years and one aged above 80 years. The male to female ratio was 1:1.64 [5].
Sharma et al also found that the ages of patients were from 6 months to 65 years in which 54% were males and 46% were females. The youngest patient with lymphadenopathy was diagnosed as Suppurative lymphadenitis and the oldest patient was diagnosed with metastatic adenocarcinoma [15]. Farooq et al reported that the mean age of the patients was found to be 32.55 years.
Most of the patients (41%) belonged to the age group 15-45 years [3]. Malhotra et al found similar results. The mean age of all the patients presenting with lymphadenopathy was 21.67 years. The male-to-female ratio of 1.2:1 was observed, with males contributing 54.7% cases and females 45.29% cases. Shrivastav et al divided cases into three groups depending on their age: Group I (0-20
years), Group II including adolescent and middle- aged patients (21-50 years) and Group III with elderly patients (>51 years).
In Group I, there was 36.98% patients with a male: female ratio of 1.22:1; in Group II total 49.11% cases and male: female ratio was 0.92:1; in Group III there were 13.90% cases with a male: female ratio of 2.55:1. Shah et al found that the range of age of patients was from 5 months to 90 years in which 60.2% were males and 39.8% were females. Farooq et al reported that 58% were males and 42% were females [4].
Site and Size- Most of the cases presented with cervical lymphadenopathy (81.6%). Generalized lymphadenopathy was seen in 1.2% of cases. Lymph nodes of > 3cm size were seen in 19.1% cases.
Shrivastav et al found that among the various sites of lymph node involvements, cervical lymph nodes were the most common (85.82%) cases followed by, supraclavicular (4.22%), inguinal nodes (3.48%), axillary (2.73%) and in (3.73%) of cases more than 1 site was involved [4].
Shah et al observed that among the various sites of lymph node involvement, maximum numbers were of the cervical region (88.5%), followed by axillary region (6.5%) and inguinal region (4.1%). 0.9% of cases showed generalized lymphadenopathy [14].
The most common site of involvement was cervical lymph nodes comprising the majority (32%) of the cases in the study conducted by Farooq et al [3]. Sharma et al noted that cervical lymph nodes were involved most commonly (84%) followed by axillary (3%), inguinal (2%) and generalized (1%) [15].
Malhotra et al observed that 39.73% of patients had solitary lymphadenopathy and 135 62.26% of patients had multiple enlarged lymph nodes. The cervical region was found to be the most common site of lymphadenopathy (71.79%) followed by axillary region (11.11%), inguinal region (6.41%), abdominal region (4.70%) and mediastinal region (1.79%).
Deep‑seated lesions were aspirated under image guidance (both computed tomography and ultrasonography). Of the 168 patients with cervical lymphadenopathy, 26.19% had sub‑mandibular lymph nodes, 9.52% had supraclavicular, and 3.57% had submental lymph nodes. The size of the lymph nodes was <1 cm in 6.41% cases, ranging from 1 to 3 cm in 78.20% and >3 cm in the


 ©
©