Study of morphological types of anemia in pregnant women with low socioeconomic status attending antenatal care at rural tertiary care hospital
Patil JD.1, Nagare MR.2
DOI: https://doi.org/10.17511/jopm.2020.i03.07
1 Jayraj Devidas Patil, Undergraduate student, MIMER Medical College, Pune, Maharashtra, India. https://orcid.org/0000-0002-5448-4472
3* Mangala Rajesh Nagare, Assistant Professor, Department of Pathology, MIMER Medical College, Pune, Maharashtra, India. https://orcid.org/0000-0001-7107-5120
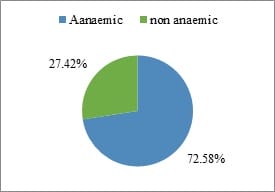
Introduction: Anemia is a major public health problem affecting both the developed(14%) as well as the developing(51%) countries. India became the first developing country to take up a National Nutritional Anemia Prophylaxis Program (NNAPP) to prevent anemia among pregnant women. Aims and objectives: 1.To find out the prevalence of anemia in ANC patients with low socioeconomic status2. To find out morphological types of anemia in this ANC patients 3.To study the various factors causing anemia in this group. Material and Methods: The type of this study is the Cross-Sectional Study, it was conducted on the ANC patients attending OPD and IPD of OBGY department at BhausahebSardesai Talegaon Rural Hospital, Maharashtra.The written consent of the pregnant women was obtained prior to the collection of the blood sample. Results: In the present study prevalence of anemia was found to be 72.58%. 15.32% of women found to be mildly anemic, 52.42% moderately anemic and 4.84% severely anemic followed by 27.42% not anemic. Conclusion: Microcytic hypochromic blood picture is predominant in the present study, it indicates there are deficient iron intake and lack of awareness about proper diet. Proper interaction, information, medication, proper diet containing all nutrients, cooking in iron utensils, fortification of food and salt with iron and birth control for proper spacing of pregnancies; such measures will go long way in improving maternal and fetal outcome.
Keywords: Anemia, Low socioeconomic group, Morphological types of anemia, Pregnant women, Prevalence
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Pathology, MIMER Medical College, Pune, Maharashtra, India. Email: |
Patil JD, Nagare MR. Study of morphological types of anemia in pregnant women with low socioeconomic status attending antenatal care at rural tertiary care hospital. Trop J Pathol Microbiol. 2020;6(3):253-260. Available From https://pathology.medresearch.in/index.php/jopm/article/view/433 |


 ©
©