Uterine leiomyomas: a demographical and clinico-pathological exploration in a rustic setup of Tamil Nadu: a comprehensive study
Sankar R.1, Kulandaivel A.2, Krishnaswamy B.3*, Viswanathan P.4
DOI: https://doi.org/10.17511/jopm.2019.i08.15
1 R. Gowri Sankar, Assistant Professor, Department of Pathology, Vinayaka Missions Kirupananda Variyar Medical College and Hospital, Salem, Tamil Nadu, India.
2 Anbu Lenin Kulandaivel, Associate Professor, Department of Pathology, Vinayaka Missions Kirupananda Variyar Medical College and Hospital, Salem, Tamil Nadu, India.
3* B. Krishnaswamy, Professor and Head, Department of Pathology, Rajah Muthiah Medical College and Hospital, Chidambaram, Tamil Nadu, India.
4 P. Viswanathan, Retired Professor, Department of Pathology, Rajah Muthiah Medical College and Hospital, Chidambaram, Tamil Nadu, India.
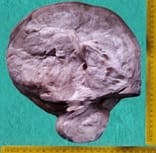
Aim: The aim of this study is to evaluate the prevalence of uterine leiomyomas in a rural setup of Tamil Nadu and also to analyse its plethora among the various neoplastic lesions of female genital tract as well as the various demographical and clinico-pathological spectrum of the same. Material and Methods: A twenty-five years retrospective study was conducted in the Department of Pathology in a rural teaching institute, Rajah Muthiah Medical College and Hospital, in Chidambaram. Result: 1200 cases were studied in the study period among the total two thousand and twenty-two female genital tract neoplastic lesions that were received in the department during the twenty-five-year period. The most common age group affected was 5th decade. The most common clinical presentation was menstrual disturbances among which menorrhagia was the commonest symptom. Taking into account the number of leiomyomas present in a uterus, single leiomyomas outnumbered multiple ones by a vast margin and taking the anatomical location of leiomyoma in a uterus into consideration, intramural leiomyoma stood well ahead of submucosal and subserosal leiomyomas. Conclusion: Almost 2/3rd of the total female genital tract neoplastic lesions received from the inception of college to December 2012 were Uterine leiomyomas there by making it the most common neoplasm of female genital tract reported in our hospital in a rural setup for a total period of twenty five years starting from the inception of college until December 2012.
Keywords: Intramural, Leiomyoma, Menorrhagia, Voluminous study, Rural Tamil Nadu
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Professor and Head, Department of Pathology, Rajah Muthiah Medical College and Hospital, Chidambaram, Tamil Nadu, India. Email: |
Sankar RG, Kulandaivel AL, Krishnaswamy B, Viswanathan P. Uterine leiomyomas: a demographical and clinico-pathological exploration in a rustic setup of Tamil Nadu: a comprehensive study. Trop J Pathol Microbiol. 2019;5(8):600-606. Available From https://pathology.medresearch. in/index.php/jopm/article/view/309 |


 ©
©