A study to assess the clinic pathological profile of patients with systemic Lupus Erythematosus
Akshatha N.1, Patil S.2*
DOI: https://doi.org/10.17511/jopm.2019.i07.14
1 Akshatha N, Assistant Professor, Department of Pathology, Gadag Institute of Medical Sciences, Gadag, Karnataka, India.
2* Shwetha Patil, Post MD Tutor, Department of Pathology, Gadag Institute of Medical Sciences, Gadag, Karnataka, India.
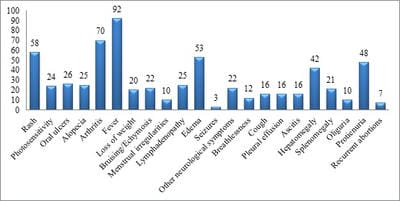
Background: Systemic lupus erythematosis (SLE) is a multisystemic chronic autoimmune disorder predominantly affecting women of child bearing age. The diverse clinical course and a high prevalence of SLE make it a major cause of morbidity and mortality especially in the younger population. Objective: To study the clinic Pathological profile of patients suffering from Systemic Lupus Erythematosus. Methodology: An Ambispective study was conducted at Kasturba Medical College and hospital, Manipal from January 2011 to December 2013. A total of One hundred twenty seven cases of SLE were classified as having SLE according to the revised American College of Rheumatology (ACR) classification criteria (1997). Results: The mean age of the study subjects in the present study was 29.85±12.61years.The male to female ratio was 1:11.7. Fever was the most common presenting symptom of the patients in the present study accounting to 92 out of total 127 cases studied (72.4%), followed by ascitis and skin rashes. Conclusion: SLE is a multisystem disorder affecting predominantly young females. Polyarthritis was the most common clinical feature. Incidence of fever was the most common symptoms followed by dermatological manifestation .Hence all the cases of SLE should be evaluated in detail for the involvement of the all the systems and its manifestations in detail to improve the overall condition of the patients.
Keywords: SLE, Clinical, Ambispective, Rheumatology
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Post MD Tutor, Department of Pathology, Gadag Institute of Medical Sciences, Gadag, Karnataka, India. Email: |
Akshatha N, Patil S. A study to assess the clinic pathological profile of patients with systemic Lupus Erythematosus. Trop J Pathol Microbiol. 2019;5(7):493-499. Available From https://pathology.medresearch.in/index.php/jopm/article/view/294 |


 ©
©